Introduction
Principles of Organic Printing
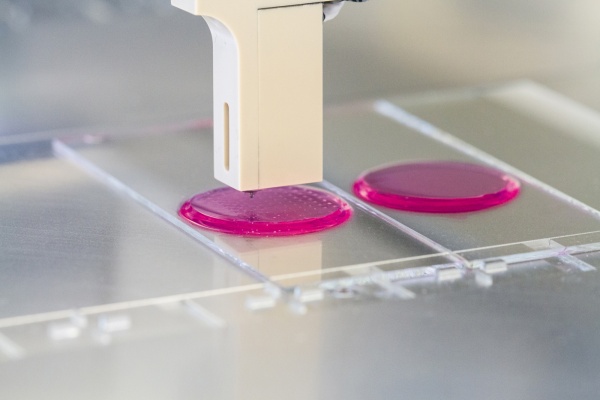
At its core, the process behind printing a 3-dimensional object is the same as printing a single 2-dimensional image. The main difference is that the final object is composed of multiple layers, each stacked on top of one another. To provide the structure for each layer, as well as for the completed organ, a biocompatible scaffold is used in many cases. This scaffold had enough space within it for the implanted cells to grow within and eventually dissolve as mature tissue fills in the blueprint that the scaffold specifies as shown in Fig. 1. In this way, each layer of the organ can be printed on the scaffold, similar to the concept of ink on paper [4].
Additionally, like different colors of ink, each layer is composed of several biological components that will eventually comprise the entire organ. Organs, by definition, are made up of multiple different types of tissue, each containing specific types of cells. Kidneys, for example, contain over 30 unique types of cells, and unless these cells are in their exact positions, the organ will not work [1]. In order to place the cells precisely, the printer contains a different cartridge and delivery needle for each cell type, which can alternate depending on the needs at the time.
All these aspects of the technology represent the current level to which scientists have developed the art of 3D printing organs. Moving forward, there are still many challenges to overcome, as well as technologies we must develop further, in order to reach the goal of printing organs customized for their intended recipients.
Advances and Challenges
The main reason that bladders have already been successfully printed and transplanted is because of the comparative simplicity of the organ. Bladders comprise two types of cells-urolithelial cells lining the exterior and interior, and smooth muscle cells providing a means to drain the organ by contraction [6]. Because of this, seeding the scaffold and getting the cells to grow properly is relatively simple compared to the challenge of predicting the growth and spread in the scaffold of the 30+ cell types present in a kidney. Each of these unique cell types grows differently in the scaffolding; printing must be very precise in terms of where the cells are placed. It is possible, however, that we will never be able to predict how tissues will grow to fill out the scaffold, so alternative printing methods are desirable for a few distinct reasons. You can find a visual of this in Fig. 2 .
Since the scaffolding is initially composed of a material like collagen that would not normally be found in the organ, it carries a risk of rejection [1,6]. Although it does degrade over time, this potential rejection coupled with the difficulty of predicting the growth of multiple types of cells in it means we should look into alternative ways of printing (See Fig. 3) . One promising technique that several groups have begun researching involves printing without the scaffold, instead relying on what are referred to as tissue spheroids for structure.
Printing with tissue spheroids is best likened to inkjet printing, wherein tiny droplets of ink are deposited on the substrate that you are printing on. In 3D organ printing, those droplets are clusters of cells mixed with some amount of growth nutrient, but there is the possibility of different inks mixing for undesirable results [2]. To prevent this, each group of spheroids, collectively known as a cell aggregate, is encapsulated in a hydrogel mold [4]. This hydrogel mold does not serve the same function as a traditional scaffold, as rather than providing mechanical stability, it provides a barrier that allows for the cell aggregates to fuse into tissues without combining. This technique would allow for printing of entire organs without the use of scaffolds, as well as a higher degree of control over how the tissues develop [3].
Some labs have already begun to experiment with this technology, and recently have been able to print vascular tissue without using scaffolding. Rather, the printer lays down layer-by-layer of these spheroids in droplet-sized portions, allowing the individual droplets to grow and fuse together, forming an aggregate [5]. In the case of printing a vascular tissue such as an artery, two concentric rings would be printed on each layer, separated by a layer of hydrogel. One ring would be comprised of endothelial cells that would make up the inner lining of the vessel, and the other ring would be comprised of smooth muscles. The individual droplets comprising each ring fuse over time, forming solid tubes of cells, before eventually the hydrogel is removed, leaving an intact vascular construct [3]. This technology of utilizing tissue spheroids to print complete organs is still years from perfection; however, although in its current state it represent a significant level of technological development in the field of tissue engineering.
Conclusion
References
-
- [1] S. Leckart. “How 3-D Printing Body Parts Will Revolutionize Medicine” Popular Science 6 August, 2013. http://www.popsci.com/science/article/2013-07/how-3-dprinting-body-parts-will-revolutionize-medicine
- [2] I.T. Ozbolat. “3D Functional Organ Printing: Promises and Future Challenges” Proceedings of 2013 Industrial and Systems Engineering Research Conference 2013. Print.
- [3] V. Mironov. “Organ Printing: computer-aided jet-based 3D tissue engineering” Trends in Biotechnology Vol. 21, No.4, 4 April 2003. http://www.sciencedirect.com.libproxy.usc.edu/science/article/pii/S01677799030003 37
- [4] T. Boland. “Cell and Organ Printing 2: Fusion of Cell Aggregates in ThreeDimensional Gels” The Anatomical Record Part A 272A:497–502, 2003. http://onlinelibrary.wiley.com/doi/10.1002/ar.a.10059/pdf
- [5] V. Mironov. “Organ printing: Tissue spheroids as building blocks” Biomaterials 30(12):2164-2174, April 2009. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3773699/
- [6] A. Atala. “Tissue-engineered autologous bladders for patients needing cystoplasty” The Lancet, Vol. 367, 9518:1241-1246, 15-21 April 2006. http://www.sciencedirect.com.libproxy.usc.edu/science/article/pii/S0140673606684389
- [7] https://www.youtube.com/watch?v=N5xQB7Rgd98
- [8] http://www.washingtonpost.com/wp-srv/special/science/how-bioprinting-works/
- [9] http://www.patheos.com/blogs/godandthemachine/2012/06/printing-a-humanbladder-and-kidney/