Treating drug-resistant epilepsy and depression seemed impossible a few years ago. However, with the advent of Vagus Nerve Stimulation, treatment of these severe types of diseases is now possible. VNS therapy is a powerful new treatment that modulates some neural structures and functions to benefit those diagnosed with drug-resistant epilepsy and depression. Powered by an implanted battery, electrodes attached to the left vagus nerve are activated to send electric pulses to the nerve. These pulses propagate into the brain, altering the synchronous neural activity that causes epileptic seizures and affecting many areas of the brain related to depression.
Introduction
Depression is a serious medical illness that affects more than 20 million people in the United States and millions more worldwide. It’s more than just feeling “blue” or “down” for a few days; it is an ongoing feeling that never leaves those with the disease. These feelings often dominate and ruin patients’ lives. There are a few options for patients with depression: medications, counseling, and now Vagus Nerve Stimulation (VNS). Antidepressants work to fight the symptoms of depression by increasing the availability of neurotransmitters, molecules that propagate or inhibit neuron-to-neuron impulses in the brain. The two most common antidepressant drugs, namely serotonin-selective reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs), increase the levels of the neurotransmitters serotonin and norepinephrine. These chemicals affect many regions and structures of the brain including centers for mood, motivation, appetite, sleep, and several other areas involved in depression [1]. However, as with all drug treatments, there are adverse side effects, which often result in patients avoiding the drugs. Furthermore, the treatments do not cover everybody; cases of intractable drug-resistant depression are on the rise. Additionally, the blood-brain barrier, a very selective membrane that prevents the vast majority of small molecules from entering the central nervous system, hampers drug research.
The other option that many patients with depression seek is counseling. Despite being very effective if used properly, counseling can be expensive and time-consuming. For the most part, depression can be treated with antidepressants, counseling or a combination of the two. However, VNS offers a more simple and effective approach; in a mechanism similar to epilepsy treatment, VNS has been found to curb the effects of depression [2].
Similar to major depression, severe forms of epilepsy can be life-altering negative experiences for patients. Epilepsy is a common neurological disease, a chronic condition characterized by spontaneous, recurrent seizures. An epileptic seizure is associated with a temporary, hypersynchronous neuronal discharge [3]. During its outbreak, millions of neurons discharge simultaneously, causing an electrical overload in the brain.
Worldwide, 50 million people suffer from epilepsy, many of whom take one or more of the 15 different anti-convulsant medications. However, the drugs have painful side effects, and 50% of people with epilepsy lack adequate seizure control or continue to have disabling side effects [4]. In fact, 20-30% of all individuals with epilepsy have drug-resistant forms of the disease. Consequently, drastic measures — such as ablative surgery in the temporal lobe of the brain — need to be adopted in these patients; otherwise, the lack of seizure control can lead to devastating psychosocial and health consequences, including serious accidents and cognitive or behavioral deterioration [2]. The advent of Vagus Nerve Stimulation has provided a safer alternative to brain surgery for the treatment of the drug-resistant form of epilepsy.
Vagus Nerve Stimulation Therapy
Vagus Nerve Stimulation is a therapeutic procedure in which electrical impulses are sent to the left vagus nerve, which then propagate into the brain. Because of direct heart innervations by the right vagus nerve, stimulation of that nerve can lead to numerous heart problems including severe bradycardia, AV block, and cardiac arrest. Thus, use of the left vagus nerve is the preferred mode of delivery [1].
The VNS therapy system consists of an implanted battery-powered electrode, which is connected to the left cervical vagus nerve. The pulse generator, with an enclosed battery, is implanted in the upper left chest. The electrode is wrapped around the vagus nerve in the neck, and wires are used to connect the electrodes to the pulse generator. The system supplies low frequency (30 Hz), recurring, intermittent, pulse electrical signals (1.0-3.0 mA, 500 μs pulse width) to the nerve [1].
The pulse generator can be programmed for the desired pulse amplitude as well as duration of the signal, as prescribed by the doctor or physiologist [4]. Typically, the VNS sends an electrical output for 30 seconds, which is followed by five minutes without output. Patients also receive a special magnet that can activate or deactivate the device if passed over the pulse generator [1]. If an epileptic patient senses the onset of an a seizure, he/she can activate the VNS, which may prevent the seizure from occurring. Shown above are both the pulse generator and the electric lead.
The VNS therapy in the United States is available for treatment of both epilepsy and depression patients. The FDA approved VNS for epilepsy in 1997 and depression in 2005. To qualify for the treatment, the minimum age requirement is 12 years for epilepsy patients and 18 for depression treatment [4].
Mechanism of Action
Epilepsy
The mechanism of action of VNS therapy for epilepsy remains largely unclear because of the complicated nature of the disease. This notwithstanding, large amounts of scientific research have yielded promising theories [4]. For instance, it is believed that the VNS disrupts the hypersynchronous electrical activity in the brain. Continual stimulation of the vagus nerve, by an implantable electrical device might result in bilateral activity of the brain circuits.
The neuroanatomical connections provide support for this theory. Sensory neuron fibers, which comprise about 80% of the axons in the cervical vagus nerve, terminate on and thus directly innervate the ipsilateral medulla and the nucleus tractus solitarius, both of which are located in the brain stem. According to Alan Guberman, positron emission studies have shown that electrical signals inputted into these nuclei are “conveyed to widespread bilateral regions of the cerebral cortex, diencephalon, and limbic system.” The activation of certain neural regions and inactivation of others is believed to disrupt the massive neural discharge that leads to epileptic seizures [2].
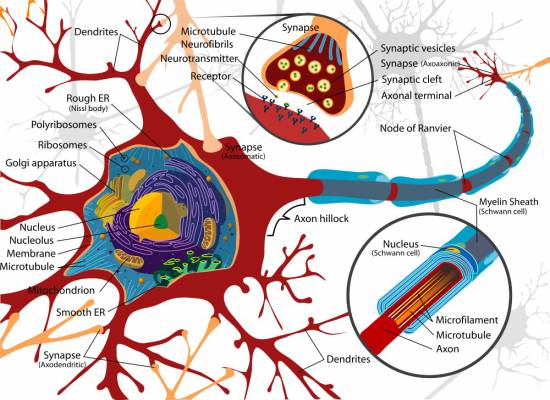
LadyOfHats/WIkimedia Commons
Figure 1: A complete neuron cell diagram.
Depression
Shortly following the approval of VNS therapy for treatment of drug-resistant epilepsy, researchers noticed an unexpected beneficial effect of the therapy. The epileptic patients felt a significant mood improvement. Further research revealed that the decrease of seizure frequency was not related to the mood improvement. This remarkable side effect opened the door for depression treatment using the VNS therapy [5].
The mechanism of action of the VNS therapy for depression is also unknown; however, it is better understood than the corresponding VNS function in epileptic patients. It is believed that the VNS therapy modulates neurotransmitters and brain structures that are thought to be involved in mood regulation. The left vagus nerve directly innervates the nucleus tractus solitarius, which is connected to areas of the brain that control mood, appetite, sleep, and motivation [1]. An electrical signal from the vagus nerve can be projected to these areas through the nucleus tractus solitarius. During the VNS therapy, the positron emission tomography imaging suggests activity in the following regions of the brain: locus coeruleus, raphe nuclei, amygdala, hypothalamus, orbitofrontal cortex, cingulate gyrus, and thalamus.
Each brain part plays a role in mood regulation and depression. Like antidepressant drugs, the VNS therapy increases the availability of neurotransmitters in the brain. Locus coeruleus is the primary source of norepinephrine-producing neurons, while the raphe nuclei are the major sites of serotonin production. The amygdala is the center for generating fear and anxiety, while the hypothalamus regulates emotions and behavior. The orbitofrontal cortex also regulates emotions, and may control the autonomic nervous system. The cingulate gyrus is involved in self-perceived conflict and response to pain. Finally, the thalamus is responsible for cooperative social behaviors. Like pieces in a jig-saw puzzle, these individual brain regions each play a role, fitting neatly into producing the overall symptoms of depression. The VNS therapy has been shown to stimulate an activity within each of these brain structures, an understanding of which provides clues for deciphering the mechanism of treatment of depression [1].
Surgical Implantation
Surgical implantation of the Vagus Nerve Stimulator is an outpatient procedure and is relatively simple from a surgical perspective. First, the surgical team makes two incisions, one in the left upper chest and the second on the left neck (cervical) above the vagus nerve. Next, a device known as a tunneler is passed through the chest incision up to the cervical opening; this will allow the wires from the electrode to the pulse generator to go neatly inside the body. With the wire put in place, the electrode with adjustable strings is then placed around the vagus nerve and is connected to the wires. Touching the electrode may damage it; therefore, the strings are used for manipulation and proper placement. A strain-relief bend is created, and the electrode is secured to the fascia. The pulse generator is then connected to the wires and placed in a deep subcutaneous tissue in the left upper chest. The incisions are closed, and the operation is complete. The patient can usually leave the hospital on the same day after the operation [4].
The pulse generator is initially set at zero amps for two weeks following surgery; afterwards, the doctor or neurologist sets the pulse generator to desired levels for adequate therapy [4].
Analysis
Advantages
The major advantages of the VNS device are the safety of the medical procedure and the durability of the device itself. Implantation of the device is a low-risk operation due to the simplicity of the surgery, usually an outpatient procedure. The device is also FDA approved for both depression and epilepsy treatment. The biggest advantages of the VNS system are the positive results it shows for patients, who are unable to cope with the side effects of drugs, or who suffer from an otherwise intractable disease that is resistant to drug treatments. Although there are very few formal studies for the VNS treatment of depression, preliminary results look promising. Finally, the VNS procedure can be ideal for patients suffering from both epilepsy and depression, which often coincide.
Disadvantages
A major disadvantage of the VNS therapy is its cost: $24,000 for the newest units [2]. The required surgery and the presence of a foreign device in the body are other disadvantages. The device must be replaced every 10 years, which requires further surgery. Another major disadvantage is that the mechanism by which the VNS elicits symptomatic relief is largely unknown. As a result, it is difficult to optimize the technology to minimize side effects, which include vagus nerve injury (i.e. during surgery) or parasympathetic over-stimulation. These are presented in Tables 1 and 2.
Conclusion
As a whole, the VNS therapy provides an alternative treatment for both epilepsy and depression. It is especially useful in providing treatment for drug-resistant forms of both diseases. Since VNS is a relatively new form of therapy, extensive data recording the long-term effectiveness is not yet available. However, initial studies on epileptic patients with the VNS implantation noted a 50% seizure reduction post-implantation, which occurred in 36.8% of patients in one year, 44.3% in two years, and 42.7% in three years. Additionally, major side effects subsided during the three year follow-up period [4]. In studies involving the VNS therapy for treatment of drug-resistant depression, most antidepressant reaction was seen in the initial phase of the treatment. The response rate in 12 months was 44.1%, while 39% of non-responders displayed improvement by 24 months.
It is remarkable that the VNS treatment is so effective with so little knowledge on its mechanism of action. The VNS system is bound to shed light on additional neural processes, opening the door for new stimulation techniques and treatments. It is expected to serve as a bench-mark for these future stimulation techniques.
References
-
- [1] “Vagus Nerve Stimulation: A New Depression Treatment Option.” MayoClinic. Revolutionhealth. Internet: http://www.revolutionhealth.com/ conditions/mental-behavioral-health/depression/other-treatments/vagus-nerve, 2007 [14 Oct. 2007].
- [2] Alan Guberman. “Vagus Nerve Stimulation in the Treatment of Epilepsy.” CMAJ, vol. 10, pp. 171-174, 2004.
- [3] Stavros Hadjiloizou and James Riviello.”Epileptic and Epileptiform Encephalopathies.” Emedicine. Internet: http://www.emedicine.com/neuro/ topic547.htm#section~author_information, 15 May 2006 [12 Oct. 2007].
- [4] Shoaib Shafique and Michael Dalsing. “Vagus Nerve Stimulation Therapy for Treatment of Drug-Resistant Epilepsy and Depression.” Perspectives in Vascular Surgery and Endovascular Therapy, vol. 18, pp. 323-328, 2006.
- [5] M.S. Nahas, Z. George, D. E. Bohning, F.A. Kozel, B. Anderson, J. Chae, M. Lomarev, S. Denslow, X. Li, and C. Mu. “Vagus Nerve Stimulation Therapy.” Neurology, vol. 59, pp. 56-61, 2002.
- [6] Vagus Nerve Stimulation. Cybertronics. Internet: http://www.vnstherapy.com/, 2007 [7 Oct. 2007].


