Current research in tissue engineering may soon offer a solution to the rising number of people waiting for livers. Recent research has shown promising breakthroughs; In June, 2010 researchers at the Massachusetts General Hospital in Boston managed to successfully transplant an artificial liver into a rat. This research also has the potential to advance other scientific processes, such as how pharmaceutical companies would be able to test drugs on extra livers instead of humans or animals. The scaffolding process, however, is not without hurdles. One major problem is that current working scaffolds come from human donors, meaning that this current process produces no net gain.
No More Organ Donations
Imagine the day when organ donors are no longer necessary. Organs, instead, would be grown, eliminating the anxiety of being placed at the end of a list, hoping to be lucky enough for an organ donation. Instead of taking livers, kidneys, lungs or any other transplantable organs from the deceased, the organs would be grown in a laboratory. Although this concept appears to have emerged from a science fiction novel, it is closer to becoming a reality than you may think. Tissue engineering may provide the answer in the near future. Researchers for the first time in June 2010 managed to artificially grow a liver in a laboratory and successfully transplant it into a rat [1]. This breakthrough is the first of its kind for tissue engineers trying to grow livers in a laboratory.
Dealing with Liver Disease
As of February 2011, over 17,000 Americans are on the waiting list for a liver transplant [2]. Last year, there were 6,300 liver transplants performed while 1,400 passed away waiting for a donor [1]. Liver disease is a serious problem in the United States; livers are only second to kidneys as the most commonly transplanted organs. A transplant is necessary regardless of the cause of liver disease: cancer, alcoholism, hepatitis, or any other of the many ailments. There is, unfortunately, currently no alternative to transplantation.
The first successful human liver transplantation was performed in 1967 by a surgical team lead by Dr. Thomas Starzl, a professor at the University of Colorado [3]. By the 1980’s, the technique had become an accepted treatment and patients had approximately a 25% chance of surviving for one year following the surgery [3]. Since then, the development of Ciclosporin, an immunosuppressant drug that helps control the adverse reaction of the patient’s immune system with the foreign liver, has reduced organ rejection and increased survival rate. Currently, 87% of all recipients will survive for at least a year, and 58% have survived for at least 15 years [2].
The Science of Growing Organs
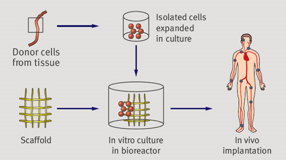
The growing list of people needing a new liver and the limited number of donors has caused a significant amount of new research in the study of materials and cells to understand tissue function and regeneration. The ultimate goal of tissue engineers is to determine an effective method for growing organs suitable for transplantation (Fig. 2). While this may seem unrealistic at this moment, researchers are having increasing success. A recent success case, for instance, is an eleven year old boy from London who received a brand new trachea grown from his own stem cells in 2010 (Fig. 1) [4]. The ability to grow organs would greatly increase the amount of organs available for transplantation and furthermore allow the organs developed to be customized to each patient’s immune system.
Researchers have achieved major breakthroughs in the past five years, with the most promising experiments managing to grow liver cells in a laboratory. In June, 2010 researchers at the Massachusetts General Hospital in Boston managed to successfully transplant an artificial liver into a rat [1]. Although the rat only survived for several hours, it was determined that the lab-grown liver was capable of breaking up toxins – the primary function of the organ. Further experimentation aims to determine methods to grow livers on a larger scale that will be accepted by the recipient’s immune system.
Growing Livers
So, how are researchers managing to grow livers in a laboratory? Several methods are simultaneously being developed, but the two most successful methods start with either a scaffold or stem cells. The scaffold is essentially a liver that has been cleansed of all the tissue, leaving just a network of blood vessels (Fig. 3) [5]. Stem cells, on the other hand, have proven extremely valuable for liver growth as they are essentially “blank” cells capable of growing into any kind of tissue.
[image=980 file=”ratliver3.png” placement=”right”]Figure 3: Rat liver after detergent is added to remove cells, leaving blood vessel intact.[/image]Researchers at Newcastle University in England managed to separate stem cells immediately after birth [6]. The stem cells are then placed in a “bioreactor,” which is a machine that regulates temperature and nutrients in the environment while giving an effect of weightlessness. This allows the stem cells to multiply faster and prepare for a transformation into liver cells. This transformation takes place after a number of hormones and chemicals are added into the bioreactor, a process that mimics how a fetus grows its own liver while still in the womb. Researchers at Newcastle have managed to grow liver tissue almost the size of a penny using this process. Since their research in 2006, however, a number of changes and modifications have been made by other groups.
In order to grow livers on a larger scale, scientists are now utilizing the potential of growing liver cells on resorbable scaffolds similar to surgical sutures. This technique involves removing a liver from the deceased and cleansing it with a detergent that leaves behind a collagen scaffold. Immature human liver cells can then be placed in the scaffold, which gives them the associated blood vessel network, providing shape and structure for growth [7]. This idea of using an organ’s scaffold has shown much promise with other organs. The doctors at the Great Ormond Street Hospital in London that operated on a ten year old boy last year gave him a new trachea developed using this technique; the organ was grown in his throat using his own stem cells and a scaffold from a separate donor [4].
Dr. Joerg-Matthias Pollok, Head of the Laboratory for Tissue Engineering and Cell Transplantation at the University Medical Center in Hamburg, Germany, has taken advantage of this scaffold technique for growing livers. He took 12 human liver cell specimens in January 2011 and placed them in a culture for two days [8]. The liver cells started to form tightly packed aggregates, known as spheroids, and started to resemble small scale livers. These spheroids were then distributed across a scaffold for further growth. Over the next two days, the number of spheroids more than doubled on average, from 18 to 41 [8]. Dr. Pollok’s experiment has offered the fastest and most efficient method for growth to date.
Such a method of using scaffolding to grow livers from specimens instead of using stem cells holds much promise. When the liver cells form spheroids, they avoid cell isolation, which allows them to be damaged during crypto-preservation [9]. Also, because the livers originate from specimens instead of stem cells, scientists avoid the controversy of using stem cells for research, which often involves destroying a fetus. Stem cells from umbilical cords provide another alternative, but that method is much more complex and expensive. Dr. Pollok claims that his scaffolding method holds enough promise, that, within five years, the laboratory may be successfully growing human livers ready for transplantation [9].
Future Possibilities
The implications of growing human livers in a laboratory hold countless opportunities for those awaiting a donor If researchers are able to successfully grow partial livers, which is a step toward growing a fully functional liver, doctors could transplant that part of the liver into patients in order to buy time for a full liver from a donor. This concept is similar to the way a dialysis machine keeps patients alive that are in need of a kidney transplant. In addition, people with partially damaged or diseased livers could receive fractional transplants as a cure instead of completely replacing a liver that is still functioning to some degree. Similarly, people with chronic liver disease could receive partial transplants over time to keep them alive instead of completely replacing their liver every few years.
The possibility of having full or partial human livers available also provides ample opportunity to pharmaceutical companies. One of the major concerns with new drugs is how the liver will react to them. If human livers are readily available, pharmaceutical companies will no longer have to partake in risky human trials that can result in accidental deaths. In addition, animal testing would become obsolete, as drugs can be tested directly on human livers without major consequence. Such valuable opportunities, however, are not yet available as there are still some major hurdles to overcome before lab-grown livers become available to the public.
Hurdles to Overcome
One of the major problems with the concept of partially transplanting livers is that there is little room to insert the new liver cells into the parenchyma, the functional part of the liver [10]. Part of the old parenchyma cannot merely be removed because the newly transplanted liver has not had time to connect and regenerate with the current liver and start functioning [11]. There must be extra room created to allow the new liver to start effectively functioning, a problem with currently no solution.
The scaffolding technique itself is also flawed. The only working scaffolds currently come from human donors, meaning there is no net gain with growing livers if a deceased human is still needed to provide a scaffold [4]. In addition, the transplanted livers cells taken from human specimens and placed into the scaffold have not been proven to survive for long in their new host due to the immune system’s rejection. Stem cells do not have this problem because they originate from the donor. Livers created from scaffolds, however, must find a different way of becoming accepted by the immune system. Perhaps, in the future, a new drug, similar to Ciclosporin, can be developed to solve this problem.
In the Future
There are clearly some major hurdles between current findings and growing functional livers in labs. The opportunities and lives saved provide great incentive, continuously pushing researchers to find a solution to the many lives lost waiting for a liver transplant. New research may even hold implications that go beyond what we expect, such as a Scottish research group that recently managed to manipulate adult skin cells into cells resembling embryonic cells [12]. This discovery provides a number of possibilities, including another way to develop liver cells in a laboratory. This could allow for a simple and effective way of creating inexpensive liver cells that may be usable for transplants, or could even provide a “cell library” that could be used to test new drugs for causing liver disease. Whatever the method, the possibility of growing human livers is becoming a reality more quickly than we can imagine, helping to heal livers and save lives.
New sentence.