Written by: Annie Lee
About the Author: Annie Lee is an undergraduate student at the University of Southern California pursuing a progressive Bachelor’s to Master’s Degree in Occupational Therapy.
Abstract
The aim of physical stroke rehabilitation is to improve motor function in paralyzed or semi-paralyzed limbs. Although the problem is physical, it begins with the brain and its weakened neurological connections to the body. Virtual reality (VR), an interactive computer-generated simulation, may prove beneficial in reestablishing the neural networks affected by stroke by training the body to respond more immediately to brain commands. According to research done at the University of Southern California, seeing a virtual avatar respond to brain signals can trick the brain into taking control over motor function again. This is due to the mirror neuron system (MNS), the part of the brain that allows us to imitate what we see. VR is a fairly new tool in the field of neurorehabilitation, but it has already proven to increase independence in daily activities, physical mobility, and even self-confidence. Its immediate positive feedback provides a more rewarding recovery experience for patients with severe strokes or other neurological disorders.
Introduction
Imagine being able to harness Jedi-like powers in an interactive virtual world—controlling objects and people with just a thought. Now, as if that were not groundbreaking enough, imagine you were a stroke victim suffering semi-paralysis on one side of your body, but now, you could miraculously move a virtual avatar’s limbs just by thinking. And more importantly, by training your brain to send the right signals to your virtual and real body through VR, you could progress to move your actual, physical upper and lower extremities again.

Welcome to 2018. Virtual reality is no longer only a trendy medium for fun and games, but also a means of restoration to an independent, meaningful life for people with disabilities. We have yet to harness telekinetic powers in real life, but mind-controlled VR has come to fruition within the past few years, and now has the potential to grant motor function to stroke patients once again.
We’ve already seen research on how embodying avatars changes real-world perspectives. For example, the National Academy of Sciences proved that taking ownership of a virtual child’s body caused people to adopt a child’s visual and spatial perspective in the real world [1]. What if we could do the same for stroke patients? Could controlling a healthy avatar allow them to embody the neurological and physical habits of a healthy person in real life? The stroke rehabilitation process normally consists of repetitive movements of paralyzed limbs, which can grow monotonous and frustration. But virtual reality allows for a more enjoyable and rewarding recovery process that not only works the body, but also the brain’s neurological networks—where the root of stroke disorder lies.
How Strokes Affect Daily Living
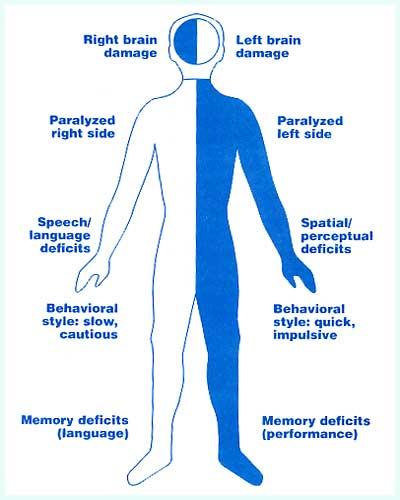
To grasp why this development is so incredible, it is important to understand what happens to your body during a stroke, and how it inhibits daily living. Stroke is one of the leading causes of adult disability in the United States, with an estimated 7 million stroke survivors today, according to the American Occupational Therapy Association [2]. Eighty percent of strokes are caused by blocked arteries (ischemic strokes), which significantly reduce blood flow to the brain [3]. Part of the brain’s networks stop working, which often causes paralysis or loss of muscle control on one side of the body and makes even simple motions, like lifting a hand, a struggle.
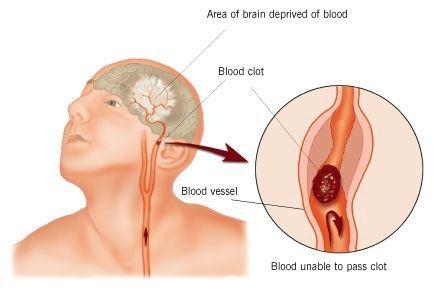
As a result, activities of daily living that the general population does without a second thought—walking, eating, and dressing—become much more complicated [3]. Signals that would normally travel at lightning-speed from the brain through the limbs slow down significantly. Other complications of stroke include decline in cognitive functioning and social disability [2]—in other words, inability to think or process social cues aptly—but much of stroke rehabilitation focuses on reconnecting the brain to the body and reestablishing motor function. Treatment often includes exercises to increase muscle strength, coordination, and range of motion. For now, we will focus on technology-assisted physical activities—specifically virtual reality—and noninvasive brain stimulation.
What Exactly is Virtual Reality?
Virtual reality simply means “near-reality.” We present our senses with fictional information, our brains process the sensory information as if it were reality, and so, our perceptions of reality change [4]. What VR looks like, practically, is a headset that with a screen that displays and immerses you in a 3D environment, eliminating any interaction with the real world. There are autofocus lens between the screen and the eyes that adjust based on eye movement and positioning. The on-screen visuals usually come from a mobile phone or a PC.
Because the phenomenon of a digitally-simulated reality is so powerful, researchers hope to apply VR in more expansive and constructive ways outside of the gaming industry. They’ve verified the benefits of VR in military training simulations through flight and battlefield simulations, and there is already a training system being fielded at Fort Bragg. [5] VR is even being used to treat anxiety through relaxation and controlled exposure to anxiety triggers. [6] Now, virtual reality technology is making a name for itself in healthcare and rehabilitation.

In the 1990s, not even the most high-profile tech companies could get VR right: Nintendo’s Virtual Boy, a 32-bit video game using a head-mounted display, became a commercial failure because of its high price and reports of user nausea; the Sega VR headset and Virtuality arcade games received similar criticisms [7]. Now, in the gleaming Information Age, the art of virtual reality has nearly been perfected. We see headsets like the Oculus Rift—a pair of VR goggles that works with desktops or laptops—as familiar gaming toys, casually accessible in retail stores and without the nasty side effects [8].
Applying Virtual Reality to Stroke Rehabilitation
Headsets like the Oculus Rift have found their homes not only in playrooms, but also in research labs like the Stevens Neuroimaging Institute at the USC Keck School of Medicine. Researcher and professor Sook-Lei Liew of USC’s Division of Biokinesiology leads a project exploring the use of VR simulation for stroke rehabilitation. Its goal: to activate damaged portions of the brain, specifically those that control movement, through the use of avatars that move in response to brain commands [9]. Liew says that after patients see their virtual arm move in response to their thoughts, “their brain activity in the motor region that [they’re] trying to target is higher, and they’re able to control the brain-computer interface a little bit better and faster.”

The MNS and Neural Plasticity Make It All Possible
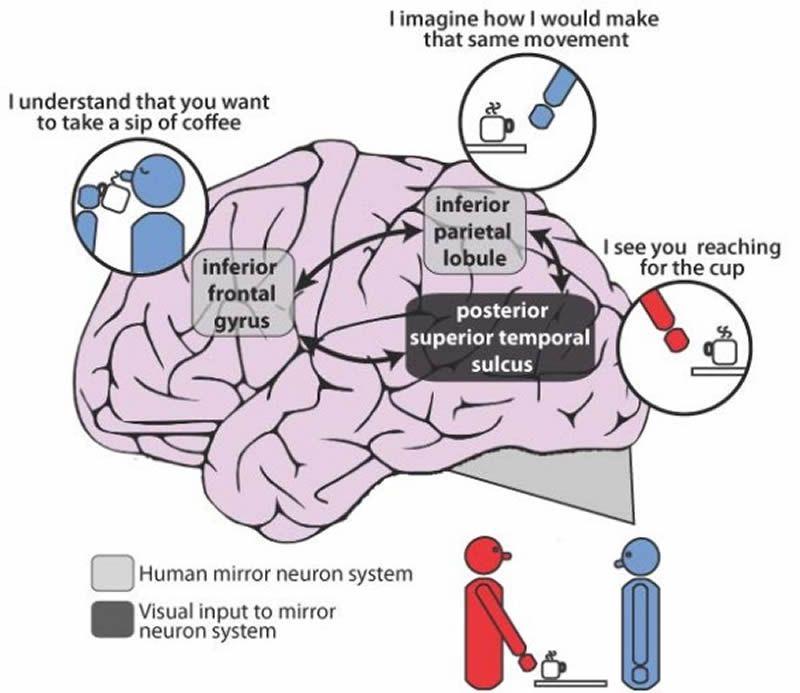
How is it possible that simply watching a virtual arm can train the mind to move our real arms? As children, we develop physical and social skills through imitation, thanks to a network in our brain called the mirror neuron system (MNS). Mirror neurons “mirror” the actions and behavior of others, and they fire when we both perform an action and merely watch someone else do that action [10]. The premise of VR for stroke rehabilitation is that merely watching an avatar move in response to one’s brain commands would activate the MNS, allowing damaged parts of the brain regain control of motor function [12].
Most people are familiar with the idea that our mind can evolve over the lifespan—our cognition and the way we think or behave—but do not realize our brains themselves and their physiological processes can be restructured. This principle is called neural plasticity, the idea that the brain can “re-program” itself and form new neural connections, including those that stimulate recovery of motor skills [13]. There is no secret formula to reorganizing the brain—it must be trained through consistent experiences, lifestyles, and environments.
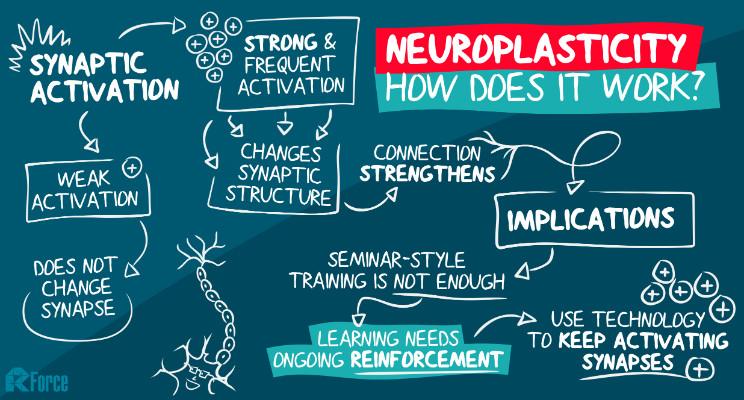
The aim of VR neural training is not only to reestablish, but to enhance two brain-body relationships disrupted by stroke: (1) the “intent before movement,” the principle that the brain must ”think” about moving before the body will, and (2) the ‘body map’, the part of our brain that processes our spacetime presence [9]. In other words, we practice getting the brain and body speaking the same language once more, so that our bodies automatically respond to brain commands again and regain spatial awareness.
Mind-Controlled Virtual Reality
So, what does this actually look like in practice? In Liew’s lab, patients don an Oculus Rift headset attached to a brain-machine interface (BMI) via 12 channels of electroencephalogram (EEG) and four channels of electro-cardiovascular (ECG) biosensors, more commonly known as electrodes. Once the electrodes are on the scalp, they make it possible for the BMI to immediately retrieve data on mental and physical reactions [11]. BMIs are direct communication pathways between an enhanced brain and an external device. Simply put, the EEGs and ECGs pick up on brain and body signals and send them to the BMI, which inputs collected data into the VR set, causing the avatar to move. This allows stroke patients to fully control their virtual limbs even without use of controllers or physical movement.

Oftentimes, stroke patients become frustrated because they do not know whether or not they’re activating the right parts of their brain when therapists ask to “think about moving” a particular part of their bodies [9]. If their limb movement is seriously inhibited, even if they’re using the right parts of their brain, they receive no rewarding feedback to tell them they’re on track. However, the VR platform’s immediate response to brain commands allows them to more clearly and quickly see the causal link between their brain and their body, alleviating frustration and speeding up recovery [9].
Positive Psychological Effects of Virtual Reality in Rehabilitation
Outside of physiological processes (i.e., the brain-body connection), virtual reality also contributes to rehab because it changes the way we perceive the world and ourselves, influencing even our emotions and thought patterns. Oftentimes, stroke patients with hemiparesis—or reduced muscle strength on one side of the body—will underuse the affected limbs, even though they still have motor function [14]. The weak brain-body connection on the affected side decreases motivation to use it regularly, and consequently, patients rely on their stronger limbs.
However, researchers at the Universitat Pompeu Fabra in Spain found a way to promote use of the neglected limb by improving patients’ confidence [14]. They asked patients to reach for targets in the virtual environment, then enhanced onscreen movement so that the patient’s limb appeared to be moving faster and more accurately than it really was. Researchers gradually increased the amplifications to keep participants unaware.
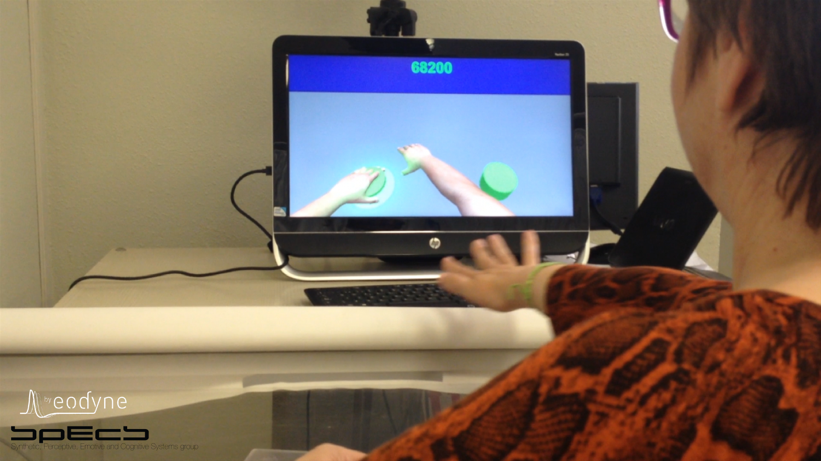
Following enhancement, patients began to use their affected limb more frequently, even choosing it over their healthy limb to reach towards a target. All it took was a boost in the patients’ confidence to overcome their hesitancy. Postdoctoral researcher and lead author of the Spanish study, Belen Rubio, says: “This therapy could create a virtuous circle of recovery, in which positive feedback, spontaneous arm use, and motor performance can reinforce each other” [14]. The mind truly reigns over matter in this recovery process.
Conclusion
Strokes are much more than an inconvenience: they’re life-altering on every level and can often lead to feelings of despair. Even if patients desire to challenge themselves physically and cognitively, their brain-body disconnection limits them. But virtual reality opens doors to a world where uninhibited movement is now within their reach. It’s an imaginary parallel world paradoxically tethered to the real one—the movement of an avatar’s limbs manipulates the brain into believing it can move the body’s real limbs.
Almost everything meaningful we do in life involves our limbs—they allow us to explore, to create, to embrace. Without them, we cannot completely take care of ourselves. But now, with the prospect of VR simulation for self-care activities and as a tool to practice motor function, restoring patients back to living their fullest, most independent lives no longer feels like a fantasy. It’s a near-reality.
References:
[1] Banakou, D., Groten, R. and Slater, M. (2013). Illusory ownership of a virtual child body causes overestimation of object sizes and implicit attitude changes. Proceedings of the National Academy of Sciences, 110(31), pp.12846-12851.
[2] Nilsen, D. (2015). Stroke Rehabilitation. [online] AOTA. Available at: https://www.aota.org/About-Occupational-Therapy/Professionals/RDP/stroke.aspx.
[3] Mayo Clinic. (2018). Stroke – Symptoms and causes. [online] Available at: https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113.
[4] Virtual Reality Society. (2017). What is Virtual Reality?. [online] Available at: https://www.vrs.org.uk/virtual-reality/what-is-virtual-reality.html.
[5] L. Mer, “Virtual reality used to train Soldiers in new training simulator,” The United States Army, 01-Aug-2012. [Online]. Available: https://www.army.mil/article/84453/Virtual_reality_used_to_train_Soldiers_in_new_training_simulator/.
[6] Wang, G. (2013). Virtual Reality Exposure Therapy of Anxiety Disorders. Advances in Psychological Science, 20(8), pp.1277-1286.
[7] Heffernan, V. (2014). Virtual Reality Fails Its Way to Success. [online] The New York Times Magazine. Available at: https://www.nytimes.com/2014/11/16/magazine/virtual-reality-fails-its-way-to-success.html.
[8] Rubin, P. (2014). The Inside Story of Oculus Rift and How Virtual Reality Became Reality. [online] WIRED. Available at: https://www.wired.com/2014/05/oculus-rift-4/.
[9] Stuart, S. (2018). How Virtual Avatars Help Stroke Patients Improve Motor Function. [online] PCMag. Available at: https://www.pcmag.com/news/359198/how-virtual-avatars-help-stroke-patients-improve-motor-funct.
[10] Rajmohan, V. and Mohandas, E. (2007). Mirror neuron system. Indian Journal of Psychiatry, 49(1), p.66.



