Abstract
Nearsightedness is a growing concern; however, new and innovative technologies now allow us to improve eyesight. In this article, we will explore corrective eye surgery, from how the eye works to how corrective eye surgeries are performed. Focusing on the latest advancement in laser eye surgery, Small Incision Lenticule Extraction (SMILE) is a quick procedure that allows people to correct their nearsightedness in the most minimally invasive way currently possible.
In 2010, roughly 2.8% of the world, about 2 billion people, were nearsighted (myopic). Experts believe that by 2050, the number of people with myopia will increase to 4.9 billion. [1], [2] Furthermore, myopia has become a prominent issue in East and South Asian countries. Rates of myopia have skyrocketed from 10-20% of the Chinese population being nearsighted in the 1950s to about 90% of Chinese children and young adults reporting to be myopic in 2015. [3],[4] As the rate of this condition is rapidly increasing and affecting the masses, this incites new and less invasive ways to correct myopia. SMILE is the newest corrective laser eye surgery procedure. Approved by the FDA in 2016, SMILE can treat myopia and astigmatism. [5]
You may be reading this article with glasses or contact lenses to correct your vision. If not, congratulations! You are one of the lucky ones. However, for those who do not have perfect vision, imagine this: you lie down for less than 10 minutes and then sit up with perfect eyesight. This is what happens when you undergo SMILE surgery.
The Workings of the Eye
The cornea, pupil, iris, lens, and retina are all parts of the eye that work together to help us see objects every day. When we see an object, light rays bounce off the object we are looking at. (See Figure 1) The light rays first enter the cornea, the outermost layer of your eye. The purpose of the cornea is to bend the light rays so the eye can focus. Next, the light goes through the pupil. The pupil is a small opening controlled by the iris, which is the colored part of the eye. It also dilates in dim light and narrows in bright light to let in the appropriate amount of light. Behind the iris is the lens. By bending to focus on nearby objects or flattening to see distant ones, the lens focuses light coming into the eye and helps us see clearly. Once the light has passed through all these layers, it is focused upside down on the back of the eye, the retina. This layer contains specialized cells called photoreceptors, which then convert the light into electrical signals. These signals are sent through the retina through the optic nerve and are sent to the brain. Lastly, the brain converts these signals into upright images that we see. [6], [7]
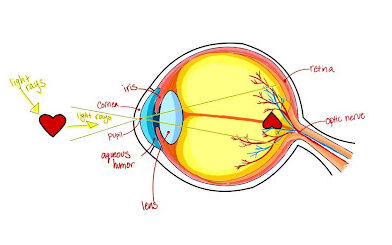
Figure 1. How the Eye Works. Adapted from [8]
Now that we understand how the eye works, we are left with the question: Which part of the eye changes to make so many people nearsighted? Myopia, or nearsightedness, occurs when the eye is elongated. A normal eye is shaped like a circle—think of a baseball —and has normal vision. However, if the eye is myopic, this creates more distance from the lens to the retina, resulting in a more “football-shaped” eye. Figure 2 visualizes the slight difference in eye shape by comparing the shape of an eye with normal vision to the shape of a myopic eye. [9] The extra distance causes the light passing through the cornea and lens to focus in front of the retina rather than on it, making distant objects appear blurry. [10]
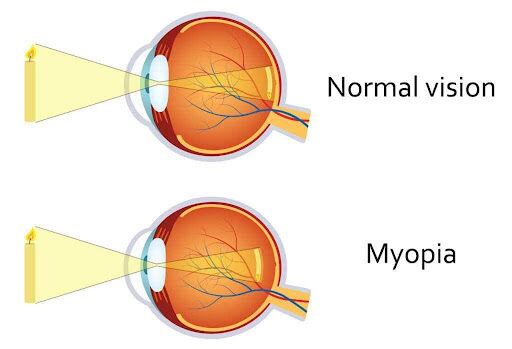
Figure 2. Normal Eye vs. Myopic Eye Visual Aid [11]
The Layers of the Cornea
The cornea is the part of the eye manipulated in any corrective eye surgery. There are five layers of the cornea. See Figure 3 for a visualization of the layers described below.
At the surface of the cornea is the epithelium, the outermost layer which makes up 10% of the cornea’s thickness. With its regenerative and resilient characteristics, the epithelium safeguards our eyes from foreign materials, and its cells renew every 7-10 days. Furthermore, the epithelium absorbs oxygen and cell nutrients from tears and distributes these nutrients to the rest of the cornea. [12], [14]
The second layer is Bowman’s Layer. This layer is composed entirely of collagen and lacks cells. This layer is not very regenerative, therefore, injuries that occur in this layer may not heal fully. As a result, scars or other irregularities could form if this layer is damaged. [12], [14]
The stroma, sandwiched between Bowman’s layer and Descemet’s membrane, makes up 90% of the corneal thickness. Composed of 78% water and 16% collagen, the stroma is strong and elastic due to its high nutrient supply. It is a supportive layer that keeps the cornea transparent which is important to let light pass through without scattering light rays. [12], [14]
Descemet’s membrane, the fourth layer, plays a crucial role in protecting the eye from infections and injuries. Made of collagen fibers, this layer acts as a barrier between the stroma (third layer) and the clear fluid (aqueous humor), and maintains proper hydration levels in the cornea. If this layer becomes damaged, there would most likely be swelling in the cornea. [12]-[14]
The endothelium is the fifth and innermost layer of the cornea. This layer’s primary function is keeping the cornea clear by regulating the hydration of the cornea and pumping out any excess fluid in the stroma. [12],[14]
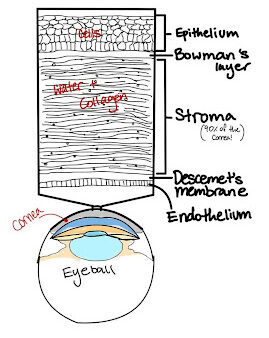
Figure 3. Diagram of the 5 Layers of the Cornea. Adapted from [15]
A Look Into the Past Of Laser Vision Correction
To best understand the history of laser vision correction, we can go back to 1948. A Spanish ophthalmologist, Jose Ignacio Barraqur Moner, performed the first corrective eye surgery. Without lasers at the time, Moner removed the patient’s cornea, dipped it in liquid nitrogen, and resculpted the stroma using a lathe. He then reattached the cornea to the patient and once healed, the patient reported improved vision. As grizzly as it sounds, his procedure worked. Moner named it keratomileusis, which means “sculpting of the cornea” in Greek. [16], [17]
Fast forward to 1988, the first laser vision correction procedure was performed. Unrelated to Moner’s procedure, photorefractive keratectomy (PRK) surgery is done by scraping off the first layer (corneal epithelium) of the cornea using a mechanical microkeratome (See Figure 4) and then reshaping the cornea using an excimer laser. Since this procedure leaves the cornea exposed, a special contact lens is placed to protect the eye during the first week of healing. Full recovery takes 2-4 weeks. While this procedure is widely successful, patients have reported pain during the healing process since this surgery removes the surface cells of the cornea. [18], [19] Despite this discomfort, many choose PRK to maintain an active lifestyle.

Figure 4. Mechanical Microkeratome. [20]
In the early 1990s, the femtosecond laser was created by Dr. Kurtz. This laser allowed corrective eye surgeons to create a small flap, called the lamellar flap, at the epithelium to expose the stroma. The femtosecond laser creates a “bladeless” way to cut the flap which has resulted in fewer flap-related complications. Using the laser to correct the stroma shape, normal vision can be restored. The lamellar flap goes almost fully around the cornea. This method was called “the Flap and Zap” technique. Since then improvements have been made regarding how surgeons would create the flap. Initially, a mechanical microkeratome (see Figure 4 for reference) was used. This device would be docked onto the patient’s eye and suctioned to cut the flap. Both methods to cut the flap are offered to patients and each has its pros and cons. In 1999, laser-assisted in situ keratomileusis (LASIK) was approved by the FDA. building on previous knowledge and results from PRK, LASIK became widely successful, with around 20-25 million procedures performed to date. [9], [20]-[22]
SMILE can be thought of as LASIK’s flapless counterpart. With comparable results of safety, efficacy, and predictability, the largest difference between LASIK and SMILE is the flap size. SMILE’s minimally invasive approach involves a femtosecond laser making a 2-5 millimeter incision along the bottom of the cornea, resembling a smiley face. Due to the small incision, patients have reported faster recovery. Additionally, SMILE is a favorable option for patients with mild dry eye, as the minimally invasive cut minimizes further drying post-operation. [5], [22]-[24]
As previously stated, the VisuMax Femtosecond Laser System was created in 2011. This machine corrects vision using precise patterns of femtosecond pulses, which have a wavelength of 1,043 nanometers and a frequency of 500 kHz. These pulses create the lenticule, the thin layer of the stroma that is extracted. There are six parts of this machine: a computer unit, laser arm, vacuum system, microscope, patient supporting system, and a foot switch. The laser is located on the laser arm. With three laser modes—“standard”, “fast”, and “expert”—the spot distance, track distance, pulse energy, and energy offset can be adjusted. The standard mode is preset by Carl Zeiss Meditec (ZEISS), the manufacturer. The fast setting can alter the laser but only by an application specialist. Lastly, the expert mode allows the surgeon to modify the laser settings depending on surgeon preferences and patient response. Though this mode is the most customizable, an application specialist is typically consulted. [25] [28]

Figure 5. Femtosecond Laser [29]
SMILE: Prep and How-To
To undergo the SMILE procedure,patients must complete multiple eye exams to determine if they are safe candidates and if their anatomy is suitable for corrective eye surgery (this exam is the same for LASIK). This comprehensive eye exam consists of six tests: a comprehensive eye exam, refractive error measurement, corneal topography, corneal pachymetry, pupil size measurement, and tear film evaluation. A candidate’s general health and medical history are taken into consideration as well before approval for SMILE. [22], [26]
The procedure itself is quite fast, reported to be 10-15 minutes long. This procedure starts with numbing the patient’s eyes using eye drops. Once numbed, an eyelid holder is placed to ensure the patient does not blink during the procedure.The suction ring is then placed onto the cornea to ensure the eye does not move while the laser shapes a small circular piece of the cornea. The laser creates the “lenticule”, which is a small circular piece of the third layer of the cornea (stroma) that the surgeon will manually extract. After the lenticule is formed, a small incision is made at the base of the cornea. The laser portion of the procedure takes about 15 seconds per eye. This incision is made for the surgeon to manually remove the lenticule which then reshapes the cornea to gain normal vision. [22], [27]
Future Implications
SMILE is a safe and effective procedure, with over 2 million procedures performed worldwide as of 2019, and technology continues to advance more rapidly than ever before. The VisuMax Femtosecond Laser System was developed in 2011, and future advancements in femtosecond laser technology could improve the precision and accuracy, as well as long-term symptoms, of the SMILE procedure. Studying how well procedure outcomes last, if patients end up needing corrective eyewear again, and any long-term symptoms, could help establish SMILE as the most reliable option for corrective eye surgery. While full recovery takes 2-4 weeks, future research and or technology can potentially cut down this recovery time to improve the experience for patients. Finally, SMILE is generally more affordable than LASIK since tonly one laser is used for SMILE. If SMILE becomes more cost-effective and accessible, it could significantly reduce the projected 4.9 million people with myopia in 2050.
Links for Further Reading:
- https://www.tandfonline.com/doi/abs/10.1080/02713683.2019.1656749
- https://www.aerzteblatt.de/int/archive/article/59189
- https://www.aao.org/education/current-insight/creating-lasik-flaps-femtosecond-laser-vs-mechanic
References:
[1] B. A. Holden et al., “Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050,” Ophthalmology, vol. 123, no. 5, pp. 1036–1042, May 2016, doi: https://doi.org/10.1016/j.ophtha.2016.01.006.
[2] “Myopia – Myopia Institute,” Myopia Institute, 2023. https://myopiainstitute.org/myopia/
[3] M. A. Bullimore, I. Morgan, K. Ohno-Matsui, and S.-M. Saw, “As Far as the Eye Can See: Importance of Myopia as a Pressing Public Health Need,” Ophthalmology Science, vol. 4, no. 1, pp. 100438–100438, Jan. 2024, doi: https://doi.org/10.1016/j.xops.2023.100438.
[4] E. S. Dolgin, “The myopia boom,” Nature, vol. 519, no. 7543, pp. 276–278, Mar. 2015, doi: https://doi.org/10.1038/519276a.
[5] Z. Dan et al, “Effects of auricular point sticking on dry eye in myopia patients after SMILE surgery: a prospective randomized controlled clinical trial,” Journal of Acupuncture and Tuina Science, vol. 19, (2), pp. 139-146, 2021. Available: http://libproxy.usc.edu/login?url=https://www.proquest.com/scholarly-journals/effects-auricular-point-sticking-on-dry-eye/docview/2918731715/se-2. DOI: https://doi.org/10.1007/s11726-021-1238-8.
[6] “How the Human Eye Focuses on JSTOR,” Usc.edu, 2017. https://www-jstor-org.libproxy1.usc.edu/stable/24989163 (accessed Feb. 24, 2024).
[7] “How the Eyes Work | National Eye Institute,” Nih.gov, 2022. https://www.nei.nih.gov/learn-about-eye-health/healthy-vision/how-eyes-work#:~:text=When%20light%20hits%20the%20retina,into%20the%20images%20you%20see.
[8] SEO Manager, “Aqueous Humor and its Role in the Eye | Fort Lauderdale Eye Institute,” Fort Lauderdale Eye Institute, Oct. 16, 2018.
https://flei.com/aqueous-humor-and-its-role-in-the-eye/ (accessed Feb. 24, 2024).
[9] “Nearsightedness San Jose | Eye Doctor Santa Clara | Spectrum Eye,” Spectrum Eye Physicians, Nov. 20, 2021. https://www.spectrumeye.com/nearsightedness-san-jose/ (accessed Feb. 24, 2024).
[10] AniMed, “How the Eye Works Animation – How Do We See Video – Nearsighted & Farsighted Human Eye Anatomy,” YouTube. Apr. 03, 2016. [YouTube Video]. Available: https://www.youtube.com/watch?v=YcedXDN6a88
[12] A. O. Eghrari, S. Amer Riazuddin, and J. D. Gottsch, “Overview of the Cornea,” Progress in Molecular Biology and Translational Science, pp. 7–23, Jan. 2015, doi: https://doi.org/10.1016/bs.pmbts.2015.04.001.
[13] J. E. Pederson and K. Green, “Aqueous humor dynamics: Experimental studies,” Experimental Eye Research, vol. 15, no. 3, pp. 277–297, Mar. 1973, doi: https://doi.org/10.1016/0014-4835(73)90147-4.
[14] S. N. Joffe, “The 25th Anniversary of Laser Vision Correction in the United States,” Clinical Ophthalmology, vol. Volume 15, pp. 1163–1172, Mar. 2021, doi: https://doi.org/10.2147/opth.s299752.\
[15] “JEC Eye Hospitals & Clinics,” JEC Eye Hospitals & Clinics Best Eye Hospital in Indonesia LASIK Cataract Dry Eye Relex SMILE Glaucoma Low Vision Retina, 2019. https://jec.co.id/en/article/cornea (accessed Feb. 24, 2024).
[16] “The History of LASIK | Journal of Refractive Surgery,” Journal of Refractive Surgery, 2021. https://journals.healio.com/doi/abs/10.3928/1081597X-20120229-01 (accessed Feb. 24, 2024).
[17] TED-Ed, “How does laser eye surgery work? – Dan Reinstein,” YouTube. Nov. 19, 2019. Accessed: Feb. 24, 2024. [YouTube Video]. Available: https://www.youtube.com/watch?v=XPDVmBg5DeE
[18] What Is Photorefractive Keratectomy (PRK, “What Is Photorefractive Keratectomy (PRK)?,” American Academy of Ophthalmology, Apr. 25, 2023. https://www.aao.org/eye-health/treatments/photorefractive-keratectomy-prk
[19] ARSC Editor, “PRK Recovery Time: What to Expect,” Refractive Surgery Council, Aug. 12, 2022. https://americanrefractivesurgerycouncil.org/prk-recovery-time-what-to-expect/
[20] S. N. Joffe, “The 25th Anniversary of Laser Vision Correction in the United States,” Clinical Ophthalmology, vol. Volume 15, pp. 1163–1172, Mar. 2021, doi: https://doi.org/10.2147/opth.s299752.
[21] K. D. Solomon et al., “LASIK World Literature Review,” Ophthalmology, vol. 116, no. 4, pp. 691–701, Apr. 2009, doi: https://doi.org/10.1016/j.ophtha.2008.12.037.
[22] M. Ang, D. Tan, and J. S. Mehta, “Small incision lenticule extraction (SMILE) versus laser in-situ keratomileusis (LASIK): study protocol for a randomized, non-inferiority trial,” Trials, vol. 13, no. 1, May 2012, doi: https://doi.org/10.1186/1745-6215-13-75
[23] J. S. Titiyal, M. Kaur, F. Shaikh, Meghal Gagrani, Anand Singh Brar, and A. Rathi, “Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives,” Clinical Ophthalmology, vol. Volume 12, pp. 1685–1699, Sep. 2018, doi: https://doi.org/10.2147/opth.s157172.
[24] D. Z. Reinstein, T. J. Archer, and M. Gobbe, “Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes,” Eye and vision, vol. 1, no. 1, Oct. 2014, doi: https://doi.org/10.1186/s40662-014-0003-1.
[25] J. S. Titiyal, M. Kaur, F. Shaikh, Meghal Gagrani, Anand Singh Brar, and A. Rathi, “Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives,” Clinical Ophthalmology, vol. Volume 12, pp. 1685–1699, Sep. 2018, doi: https://doi.org/10.2147/opth.s157172.
[26] “Preoperative Evaluation for LASIK Surgery – EyeWiki,” Aao.org, Jan. 07, 2023. https://eyewiki.aao.org/Preoperative_Evaluation_for_LASIK_Surgery
[27] I. Small, “What Is Small Incision Lenticule Extraction?,” American Academy of Ophthalmology, May 17, 2023. https://www.aao.org/eye-health/treatments/what-is-small-incision-lenticule-extraction#:~:text=With%20SMILE%2C%20your%20ophthalmologist%20uses,both%2C%20to%20improve%20your%20vision.
[28] Ekktet Chansue, Morakot Tanehsakdi, Sukanda Swasdibutra, and C. McAlinden, “Efficacy, predictability and safety of small incision lenticule extraction (SMILE),” Eye and vision, vol. 2, no. 1, Aug. 2015, doi: https://doi.org/10.1186/s40662-015-0024-4.
[29] C. Verges, “Lasik or FemtoLasik: what are their differences?,” Área Oftalmológica Avanzada, May 27, 2020. https://areaoftalmologica.com/en/blog/myopia-operation/lasik-or-femtolasik/ (accessed Feb. 24, 2024).



