What if a text message could save a life? Dr. Ayogdan Ozcan and his team of researchers have developed a cost-efficient, revolutionary device that can perform basic diagnostics for blood cell count, malaria, and tuberculosis – all on the back of a $30 camera phone. The device uses a lens-free imaging technique known as LUCAS, which creates a holographic image of each sample cell based on their imaged “shadows”. The shadows are imaged by diffracting a light beam through the cells and upon a CCD chip, which collects the data for advanced image processing. These holograms can then be compared to a holographic cell database using a simple pattern-matching algorithm that counts the cells and diagnoses any potential diseases. The diagnostic results are sent back via text message to the original patient or doctor in a matter of minutes. This device is revolutionizing the fields of microscopy and mobile health technology and may one day turn the cell phone into an essential local and global medical device.
Introduction
Imagine if you could perform a complete blood cell count and diagnose deadly bacterial diseases – on the back of your cell phone. Well, imagine no more.
An inexpensive, lightweight device is now being developed that will allow doctors and health workers to do just that: perform basic medical diagnostics on the back of a $30 cell phone. This camera phone attachment is a small digital microscope that, costing under $10 to produce, can perform many medical tests that normally require expensive lab equipment and trained personnel who can conduct tests such as blood cell count, identification of diseased cells, water contamination detection, and diagnosis of infectious diseases, including malaria, cholera, and tuberculosis (TB).
It is a lightweight, cost-effective, and lens-free microscope that uses computer algorithms instead of expensive and bulky lenses to extract an extensive set of biological information from simple, camera phone images.
The Global Cell Phone Network
Twenty years ago, a cell phone could do little else besides make a phone call. Today, however, the cell phone has become the Swiss Army knife of modern technology. Few phones are without Internet access, accelerometers, global positioning systems (GPS), or video cameras. It comes as no surprise, then, that the cell phone is now being retooled into a medical device as well.
What is surprising, however, is the ubiquity of cell phones. Today, nearly 5 billion people around the world own a cell phone [1], a majority of whom live in resource-poor countries such as Uganda and India (Fig. 1). Almost 90% of the world’s population is covered by a mobile network, and by 2015, it is estimated that 90% of the world’s population will carry a network-subscribed cell phone [2]. As Professor Ramesh Raskar of the Massachusetts Institute of Technology Media Labs notes, “People who make a dollar a day have a cell phone, which is just mind-blowing if you think about it [3].” These statistics alone make it one of the most accessible resources for innovation and healthcare intervention.
Dr. Aydogan Ozcan and his team of researchers at the Electrical Engineering lab in the University of California, Los Angeles (UCLA) have figured out a way to tap into this substantial resource and provide healthcare to the masses with a revolutionary, lens-free cell phone attachment that can bring effective diagnostics to parts of the world that cannot access expensive clinical equipment and laboratories.
The Inner Workings of A Revolutionary Mobile Device
LEDs, CCDs, and Diffraction Signatures
The device is composed of two key hardware components: a light-emitting diode (LED) that illuminates the sample and a charged-coupled device (CCD) chip, identical to that found in a consumer digital camera. Slides containing a blood or water sample are loaded into the phone in between the LED and the light-sensing chip, “just like you insert a memory stick [4],” says Ozcan. Each slide is then illuminated by the LED from above; as the light passes through the given cell type, it diffracts or bends in a characteristic way. “What we record is not an image but a diffraction signature,” says Ozcan [5]. Each cell type has a unique diffraction signature based upon its size, shape, and refractive index [5].
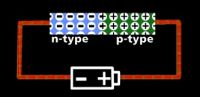
The CCD chip then collects the diffraction signatures through capacitance, the ability of electrical devices such as the chip to store energy—in this case, the diffracted light waves. Capacitance in the CCD chip operates via the gathering of electric charge, or electrons. The chip is made up of an array of light-sensitive pixels, or CCD gates, which are composed of perpendicular strips of transparent electrode material—silicon dioxide—and n-type silicon channels (n-Channels) embedded within a p-type silicon substrate [6] (Fig. 2). N-type silicon is a semiconductor capable of providing extra electrons, which the p-type silicon, normally electron-deficient, can accept and store. Points at which the n-channels cross the electrode material are known as CCD gates and correspond to one pixel.
When a photon of light strikes a particular gate, it dislodges electrons from the n-channels, which causes the formation of potential barriers and wells within the p-type substrate. The excited electrons remained trapped in these wells, and each gate begins to accumulate an electric charge in proportion to the intensity of light at that gate. Once the image exposure is complete, the CCDs operate as a shift register and transfer collected charges to the end of the column for conversion and digitized imaging [7].
LUCAS and Digital Holography
The CCD chip is part of the underlying technology behind the device known as LUCAS: Lens-free Ultra-wide field of view Cell monitoring Array platform based on Shadow imaging. Instead of directly imaging and magnifying cells with a lens, as a conventional microscope does, LUCAS uses the interferometric, or electromagnetic wave-based, technique to image cell shadows in a process known as digital holographic microscopy [8]. Unlike the dark shadows of the macro-world, such as our own, the shadows – or diffraction signatures – of micro-objects, like that of a cell or bacterium, contain an extremely rich source of quantified information that accurately describes the object’s spatial features [9]. These micro-scale shadows are not flat, but rather, rippled in texture, the details of which constitute a holographic image of the cell [10]. This hologram acts as the cell’s fingerprint and can be used to detect the cell type and potential deformations such as sickle-cell anemia and malarial disease.
Text Messages and Algorithm Matching
The holographic images are often blurry and pixilated [5]; despite their low quality, however, the images contain all the information necessary for simple software to identify and count the cells. With image processing software, the hologram can also be used to reconstruct a microscopic image of the cell. A USB port carries the data between the device and the cell phone, where it can then be sent wirelessly to a computer station for advanced image processing.
Powerful software is able to undo any cell image overlap and, through digital computation, retrieve an exact image of the cells. “We compensate for everything in the digital regime,” says Ozcan. A pattern-matching algorithm based on cell morphology then compares the images with a cell library. Dr. Ozcan created this library of holographic cell and bacterial images, or diffraction signatures, including all possible cells and bacteria to be analyzed. Based on this image comparison, the cells in the sample are counted and identified, both for type and potential deficiencies or differences that indicate infection. Once the algorithm has analyzed the sample, a diagnosis is automatically text-messaged back to the original cell phone user.
All of this happens within minutes. Currently, software that can perform the pattern-matching algorithm directly on the cell phone is being developed, which would eliminate the need to send it to a computer station and make the process even faster. In addition, researchers are working to improve the quality of images on both the hardware and software fronts; as Ozcan says, they hope to soon have “a decent enough resolution to show subcellular features.”
Differential Interference Contrast
Ozcan and his team have also constructed a version of the microscope that uses differential interference contrast, a technique used in conventional microscopes to enhance image contrast. Before the LED light beam illuminates the sample, a prism is used to split the light into two beams, each with a different polarization, or orientation in space. After the two beams pass through the sample, a second prism is used to recombine the two beams, producing a single image with enhanced edge contrast. In effect, two images of every cell, each of a different perspective, are generated, processed, and recombined to produce a single holographic image with increased contrast. This technique allows the microscope to successfully image certain strains of bacteria that are otherwise transparent to the microscope without the use of a stain.
In contrast to the $1000 it normally costs to add prisms and differential interference contrast abilities to a conventional microscope, this method costs only $3 extra to be included in this revolutionary device.
Uses and Specs
The device can be used to perform basic diagnostics such as red, white, or complete blood count, diagnosis of infectious diseases such as malaria, TB, or cholera, CD4 T lymphocyte counts for HIV/AIDS patients, diagnosis of anemia or sickle-cell disease, and water contamination tests, among others.
It weighs just 46 grams and measures about six centimeters high and four centimeters on each side. Despite being small and lens-less, the microscope is able to go submicron in terms of accuracy and specificity and can gain a resolution of about two micrometers, equal to a conventional 40X microscope. The software is fast, accurate, and has high throughput: it can image over 100,000 cells in a 20-centimeter squared field of view in just one second [5] – with at least a 90% accuracy rate. As Ozcan notes, “What most excites me about this technology is the speed that it enables… it can look at literally millions of cells per second, all with the holographic resolution that we want [11].”
The Future Potential of Mobile Microscopes
In a world in which the average flow cytometer costs around $70,000 and an advanced microscope can cost upwards of $200,000, expensive lab equipment and diagnostics are simply not an option for resource-poor countries, especially those in which a majority of the people are making under a dollar a day. Unfortunately, it is often these same countries that are most plagued by infectious diseases and water contamination: an estimated 4 million people per year die of contagious infections such as HIV/AIDS, malaria, and TB, and 6 million die from poor drinking water-related problems [11]. These countries need a cost-efficient and effective means of performing the many basic medical tests that their citizens require.
In the last few years, Dr. Ayogdan Ozcan and his UCLA research team have come to the rescue with a device that, capitalizing upon the ever-expanding, global tech-infrastructure of the mobile phones, can perform basic diagnostic tests on the back of a simple camera phone. Essentially, Ozcan figured out a way to hack into a $30 cell phone, slide in a blood sample, shine an LED light, capture a holographic image, and send out a text message that, when processed and compared to a cell library, can be used to form an almost instantaneous diagnosis of the disease.
Though made with the intention of solving global health issues, the device may soon also be found in the homes of Americans. Its ability to count white blood cells and infectious cells, for example, may be instrumental in helping doctors monitor patient response to chemotherapy – all in the comfort of the patient’s own home.
Whether or not patients adopt mobile diagnostics at home, this simple and cost-effective device is quickly revolutionizing the field of microscopy, diagnostics, and digital imaging. Who knows what the future holds. It may just be that soon, bulky, expensive microscopes will become obsolete, and the cell phone, in ranks with the stethoscope and thermometer, will become one of the greatest medical devices of our time.