Abstract
The introduction and mainstream development of infant incubators has significantly impacted the life expectancy of babies that are born as early as 24 weeks into a pregnancy [1]. Despite the high infant mortality rate in the late 19th and early 20th centuries, many medical professionals were hesitant to adopt incubator technology until Martin Couney, a circus showman from Germany, revealed the astounding survival rates that incubators provided [2]. Neonatal incubators utilize innovations such as air pressure control, heat circulation, and humidity control from a variety of engineering fields that help replicate the complex conditions that a child would experience in their mother’s womb.
Introduction
At the turn of the 20th century, patrons of New York’s Coney Island amusement park stumbled upon a fascinating new exhibit. Tucked away among the flashing lights and carnival games was the world’s first neonatal intensive care unit (NICU) [2]. Upon admission, patrons of the park would enter a sterile tent and marvel at Martin Couney and a team of nurses tending to dozens of premature infants held in strange metal contraptions to “incubate” the babies to health [2]. The show’s popularity drew attention to the potential benefits of incubators and played an important role in their acceptance by mainstream medicine. Created purely as an exhibit, incubators became an integral part of medical practices needed to nurse premature babies to health.
Over the last hundred years, the neonatal incubator has been one of the most influential contributions to the decline in infant mortality rate. Incubators are primarily used for children born as early as 6 months into a pregnancy, providing conditions similar to those in the womb [1]. Modern incubators utilize advanced microprocessors to monitor, control, and maintain the baby’s environment. These controlled factors include warm temperature, temperate humidity, safe levels of light and sound exposure, and higher-than normal oxygen levels. By providing these conditions, the potential health risks associated with premature birth, such as respiratory failure, lack of body temperature regulation, and vision or hearing loss, are minimized [1].
While its goals are simple, the modern incubator’s development since its days in the circus is a successful convergence of many aspects of engineering. Within these apparatuses are heaters operating on central concepts of thermodynamics. Fluid flow controls the humidity of the chambers, while gas exchange and partial pressure regulation ensure that the baby receives adequate oxygen and fresh air [3]. This network of systems is powered and regulated by cutting edge electrical mechanisms [3]. By integrating ideas from these disciplines, engineers have successfully created living conditions that are essential for healthy premature development.
History
In the early 1900’s, parents of premature infants from all over the country faced a difficult decision: attempt to care for their vulnerable child at home or take them to the circus. There, they would surrender their newborn to Martin Couney, who would display the baby in a glass incubator for the entertainment of paying onlookers [2].
While the infant expositions seem ethically questionable by today’s standards, the incubators at Couney’s popular sideshow were responsible for saving over 6,500 lives during 3 decades of operation, boasting a survival rate twice as high as the national average for premature infants [4]. Situated between peep shows and animal habitats in the bustling circus, Couney created fully functional NICUs with a strong emphasis on sterility and professionalism [2]. The exhibits featured doctors and nurses tending to the incubated infants around the clock while guests were welcome to visit and admire their work [2]. As word spread about the sideshow’s work, more parents brought their babies to Coney Island knowing that their child’s chances of survival were surprisingly higher in the circus than in a hospital [2].
When first introduced, most of the medical community was skeptical about the incubators’ efficacy or necessity. Many doctors at the time used their belief that premature children were “weaklings” to justify why incubators were unnecessary, and that the children couldn’t (or shouldn’t) be saved [5]. Couney made it his life’s work to prove that the incubators saved lives and kept up his operation until Cornell Hospital in New York opened the first premature infant station in 1943 [5].
Couney’s showmanship, popularity, and high success rate played an important role in the mainstream acceptance of modern incubator technology. This community support encouraged advances in the technology, progressing to save millions of newborn lives each year and more than doubling the survival rate of premature infants over the last century [6].

The Inspiration for Couney’s Incubators
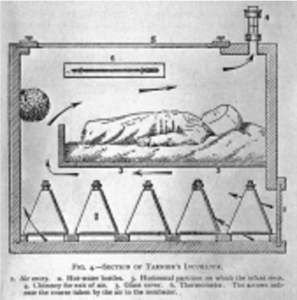
The application of the incubator to human healthcare was first developed by French obstetrician Étienne Tarnier [8]. Inspired by the technology used for keeping young chicks warm, Tarnier’s incubator consisted of insulated walls and a thick glass cover to allow for easy monitoring of the chicks by nurses. The interior was kept near body temperature level by warming and circulating air through the chamber, using mechanisms similar to the thermodynamics of a convection oven. Fresh air entered through a port below the baby and exited through a small tube in the top of the box to minimize exposure to contaminants [9]. A thermometer inside of the box allowed caretakers to measure and alter heat and air flow without opening the device (Figure 2). After noticing the design at the 1896 World’s Fair, Couney immediately saw the potential of Tarnier’s incubators and brought them to America at the turn of the 20th century [10]. The showman opened his two incubator exhibits in Coney Island using this design [8].
Current Technology and Important Parameters
Several modern designs of neonatal incubators have emerged, all of which are great additions to neonatal care. For instance, the GE Giraffe Omnibed is an example of a typical modern neonatal incubator design (Figure 3) [11]. Incubators like the Omnibed have the ability to provide oxygen, humidity, and temperature control while also alerting staff if any significant changes to these conditions arise [11].
Over time, neonatal incubators have progressed from gas to electrical heating. The newest forms of these devices are controlled by a microprocessor. This small chip with complex integrated circuits allows for easy and precise manipulation of the incubator’s controls without occupying the large amount of space that traditional circuitry might within the machine [11].
Unlike the incubators of Martin Couney’s day, many of the environmental parameters are adjusted without the need for human intervention. Microprocessors have the ability to control temperature, humidity, oxygen, and light by using sensors which can be calibrated to alert nurses or physicians when the environment reaches certain high or low thresholds and will automatically adjust the parameters accordingly [3]. For example, a thermometer near the infant is able to sense any significant changes in temperature, which the microprocessor would use to alert medical personnel while recalibrating the electrical signals to the heating system. This leads to a rise or fall in temperature until it reaches a desirable state.

Temperature
The primary purpose of incubators is to emulate the thermoregulation of the womb that premature infants are unable to control themselves. By using reflective materials and convective technology to evenly heat the baby from all sides and allow access from 3 of the 4 walls, the device maintains an internal temperature between 28-39o C to keep the infant’s temperature at a standard level (37o C) [11,12]. Thus, doctors are able to perform medical procedures, change diapers, or handle the baby without compromising the delicate environment that the newborn requires [12]. The convection of air produced by an electric heater creates a uniformly heated environment either passively through natural air currents or actively by a fan associated with the heater [13].
Humidity
Humidity plays an important role in maintaining the baby’s internal temperature as well as their environmental sterility. If humidity levels are too high, the patient risks becoming a breeding ground for germs and bacteria [3]. If too low, the dry climate can cause dehydration and cooling of the body temperature due to evaporation on the skin [3]. Modern incubators produce and maintain a humidity level between 40% and 75% by heating and evaporating water in an attached reservoir [11]. The amount of heat applied to the reservoir is directly proportional to the amount of moisture in the incubator’s atmosphere.
Light and Noise
Sensory input from stimuli can affect the central nervous system and reduce REM sleep, which is critical for healthy growth and development [14]. Many NICUs are designed to promote normal sleep patterns and reduce circadian disturbances by providing regular light and dark cycles [3]. Light and noise levels are also regulated by the walls of the box, which provide insulation from most noise penetration and often contain photo sensors to detect whether the baby is being exposed to unwanted levels of light [12]. Too much UV exposure can cause serious retinal damage during early stages of human development and many premature births lead to this complication, making light an important factor to consider. design [1].
Oxygenation
In many cases, premature infants have respiratory issues caused by incomplete organ development at the time of birth [3]. To ensure adequate oxygen delivery, incubators have the ability to directly regulate the amount of oxygen that the baby is exposed to. The concept is similar to assistive tanks required for patients with severe respiratory illness. In these cases, air is delivered at a fixed rate from a tank through a tube directly connected to the nostrils. This direct connection increases the partial pressure of oxygen in the lungs and allows for more oxygen to diffuse into our bloodstream, an important process for maintaining normal body function. Rather than exposing the infant to potential risks associated with a direct connection to a breathing apparatus and potential tangling with the tubes, the internal partial pressure of the gas is uniform throughout the incubators [3]. By maintaining a high level of oxygen which can be automatically adjusted via microprocessor, the baby is able to receive more oxygen than normal atmospheric conditions can provide [3].
The Future of Neonatal Care
While the current technology for neonatal incubators is currently highly effective in saving the lives of premature babies, the field is constantly changing due as new studies on fetal development are published. For example, an article by TK Ferris and MM Shepley discusses the importance of reducing the amount of auditory and visual exposure that the newborns receive [14]. This would encourage more improvements on the filtering of the noise and light on the device, creating better results. In addition to working on expanding the technology within the incubators, a human centered approach to the design is also important[14]. This would involve tailoring incubators and NICUs in a way which is more intuitive for hospital staff to use, leading to a reduction in caretaking mistakes and improvement in the satisfaction of the newborns’ parents [14].
Conclusion
Although he was initially disregarded by the medical community, Martin Couney’s infant circus sideshow attracted attention from the world, saved dozens of lives, and paved the way for the widespread acceptance of NICU technology. The neonatal incubator is a feat of engineering with a fascinating history and astoundingly positive effects on the reduction of child mortality. While its basic structure and function have remained constant over the past century, the precision and efficacy of the device continues to evolve as our engineering abilities progress. By bringing together mechanical, electrical, chemical, and systems engineering discoveries to make this technology work, the design of incubators can be appreciated by members of nearly every scientific discipline.
References
[1] K. Danielsson, “Premature Birth and Survival Statistics,” Verywell Family, Jan. 19, 2020. [Online]. Available: https://www.verywellfamily.com/premature-birth-and-viability 2371529 . [Accessed Mar. 1, 2020]
[2] R. F. Snow, “American Characters: Martin Couney,” American Heritage, vol. 32, no. 4, Jul, 1981. [Online] Available: https://www.americanheritage.com/martin-couney. [Accessed Mar. 2, 2020]
[3] H. Mittal, L. Mathew, A. Gupta, “Design and Development of an Infant Incubator for Controlling Multiple Parameters,” International Journal of Emerging Trends in Electrical and Electronics, vol. 11, issue 5, Sep. 2015. [Online] Available:
https://pdfs.semanticscholar.org/c72d/04ca75b186904fc7904d2c7354334e23bf5b.pdf. [Accessed Mar. 3, 2020]
[4] J. P. Baker, “The Incubator and the Medical Discovery of the Premature Infant,” Nature Journal of Perinatology, vol. 20, no. 5, pp. 321-328, 2000. [Online]. Available: https://www.nature.com/articles/7200377.pdf?origin=ppub. [Accessed Mar. 1, 2020]
[5] R. Barry, “Coney Island’s Incubator Babies,” JSTOR Daily, Aug. 15, 2018. [Online]. Available: https://daily.jstor.org/coney-islands-incubator-babies/. [Accessed Feb. 28, 2020].
[6] E.A. Reedy, “Care of Premature Infants,” Penn Nursing. [Online] Avaliable: https://www.nursing.upenn.edu/nhhc/nurses-institutions-caring/care-of-premature infants/. [Accessed Mar. 3, 2020]
[7] A. Burgess, “When Infants in Incubators Were a Sideshow Attraction,” Atlas Obscura, Sep. 27, 2020. [Online] Available: https://www.atlasobscura.com/articles/infant incubator-coney-island. [Accessed Mar. 2, 2020]
[8] E. Blakemore, “Baby Incubators: From Boardwalk Sideshow to Medical Marvel,” History Channel. A&E Television Networks, Sep. 12, 2018. [Online]. Available:
https://www.history.com/news/baby-incubators-boardwalk-sideshows-medical marvels. [Accessed Feb. 26, 2020]
[9] P. Budin, “Section of Tarnier’s incubator,” The Nursling, 1907. [Online] Available: https://wellcomecollection.org/works/bdapc3tb?wellcomeImagesUrl=/indexplus/image /L0005632.html. [Accessed Mar. 2, 2020]
[10] “History of Medicine: The Incubator Babies of Coney Island,” Columbia University Irving Medical Center, 2019. [Online] Available:
https://columbiasurgery.org/news/2015/08/06/history-medicine-incubator-babies coney- island. [Accessed Feb. 28, 2020]
[11] M. Abdiche et. al., “Humidity control tool for neonatal incubator,” Medical and Biological Engineering and Computing, Apr. 1998. [Online] Available:
https://www.researchgate.net/publication/13601630_Humidity_control_tool_for_neon atal_incubator. [Accessed Apr. 27, 20200
[12] “Neonatal Incubator,” ScienceDirect. Elsevier B.V. 2020. [Online]
https://www.sciencedirect.com/topics/nursing-and-health-professions/neonatal incubator. [Accessed Feb. 28, 2020].
[13] “Thermal Control of the Newborn: A Practical Guide,” World Health Organization, Geneva, Switzerland, 1993. [Online] Available:
https://apps.who.int/iris/bitstream/handle/10665/60042/WHO_FHE_MSM_93.2.pdf;se quence=1. [Accessed Mar. 3, 2020]
[14] T.K. Ferris, M.M. Shepley, “The design of neonatal incubators: a systems-oriented, human-centered approach,” Nature Journal of Perinatology, vol. 33, pp. 24-31, 2013. [Online]. Available: https://www.nature.com/articles/jp201311.pdf?origin=ppub. [Accessed Feb. 28, 2020].
[15] “GE Giraffe OmniBed,” Soma Tech Intl, Jan. 15, 2020. [Online] Available: https://www.somatechnology.com/Incubators/GE-Giraffe-OmniBed.aspx. [Accessed Mar. 2, 2020]




